This is a chapter from #PRstack: AI tools for marketing, media, and public relations, the latest #FuturePRoof publication. You can buy a copy of the complete book from Amazon in Kindle and print formats. The Kindle version doesn’t include images due to format limitations.
Propel by Zach Cutler | Developer
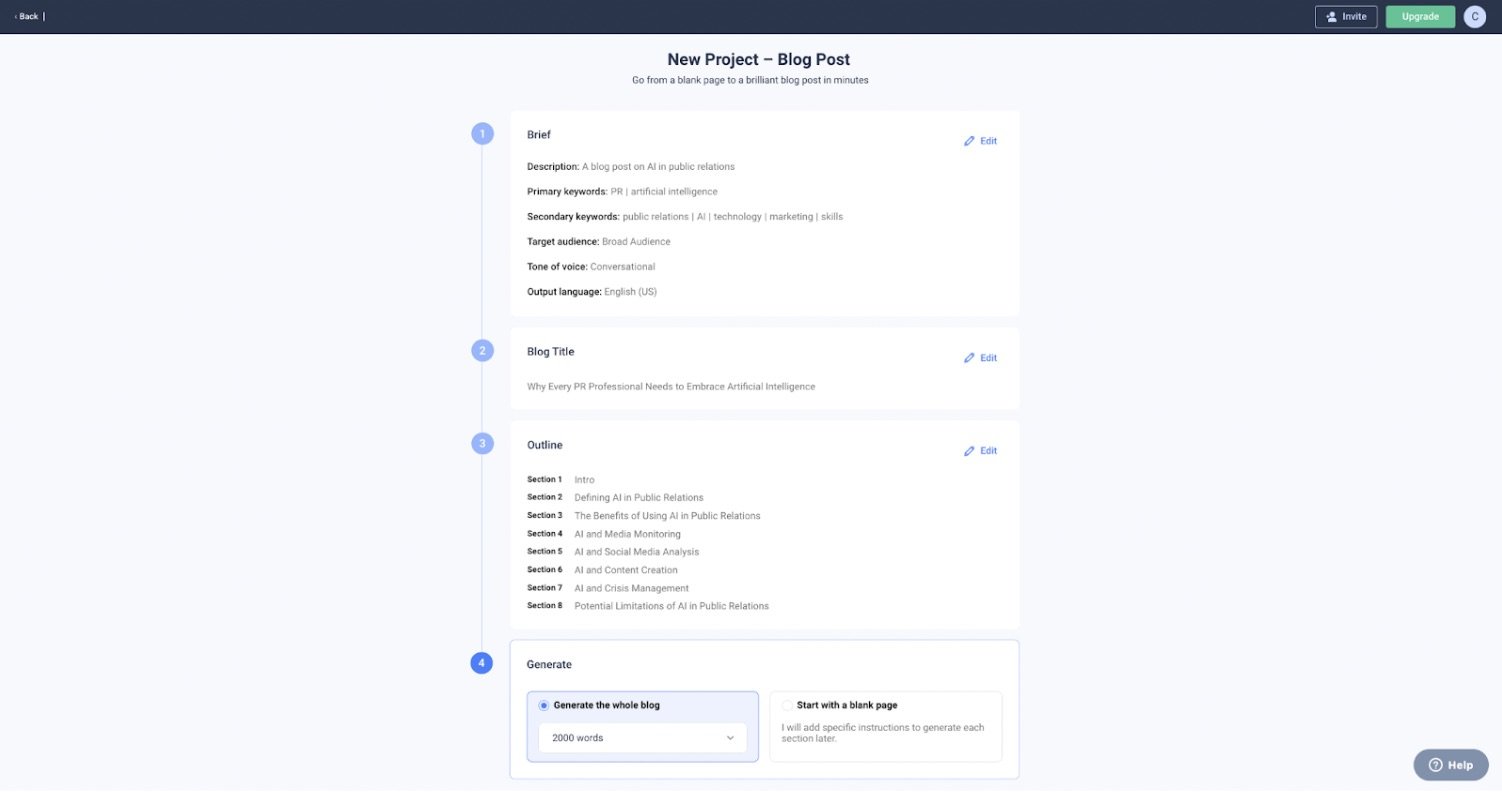
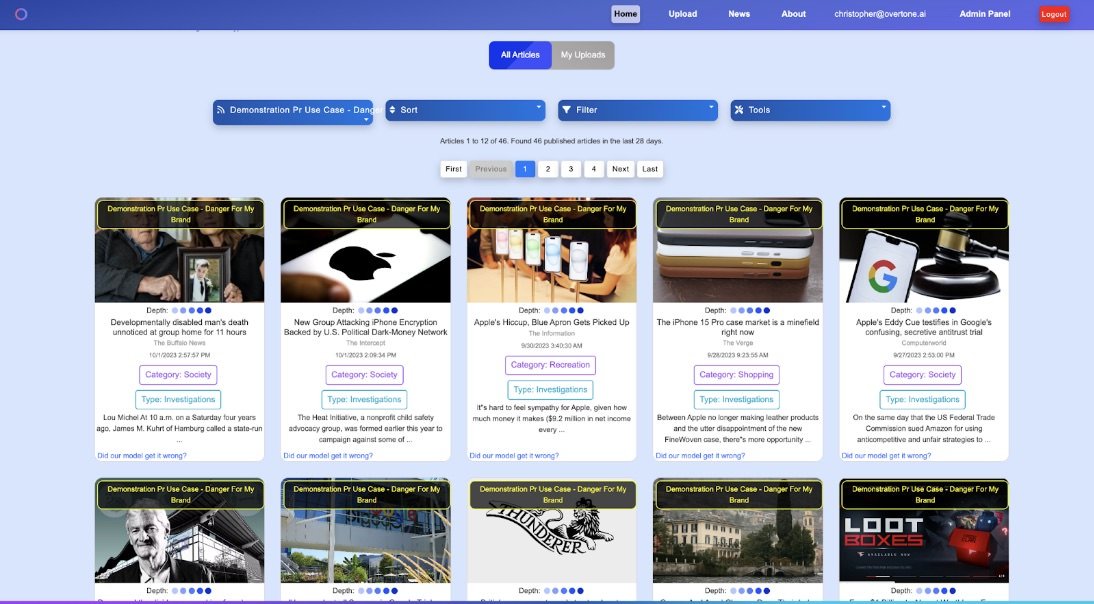
Propel is a leading AI-powered Public Relations Management (PRM) tool. Propel enables agencies and in-house teams to generate content, discover media targets, pitch stories, monitor coverage/ROI and win at earned media. Features include a full CRM for media relations, Gmail and Outlook plugins, a generative AI powered suite, media monitoring service, and business outcomes indicator.
Where it fits within public relations workflow
Propel PRM fits into every part of the public relations workflow, from finding journalists to pitch to showing how well campaigns are going - both in terms of coverage and bottom line. The PRM manages the entire flow from pitch to publish; from gen AI pitch and press release writers and media list management to sales funnel metrics resulting from successful placements in publications. Propel’s platform can touch every piece of the typical communications workflow, streamline it, and make it more organised. In short, it automates and simplifies the mundane, time consuming aspects of media relations practice so that practitioners can focus on messaging, play down strategy, and build journalist relationships.
How to use it
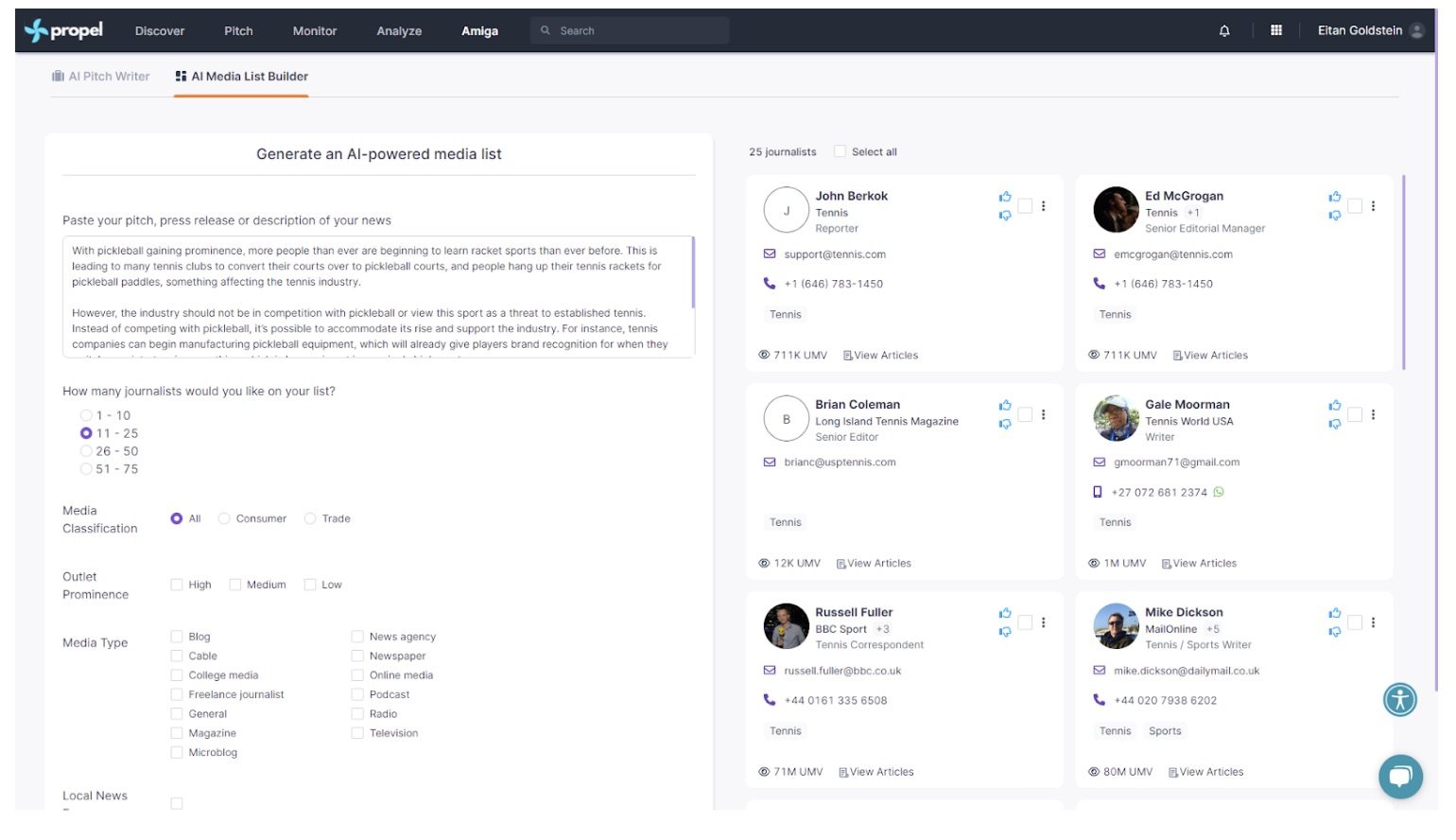
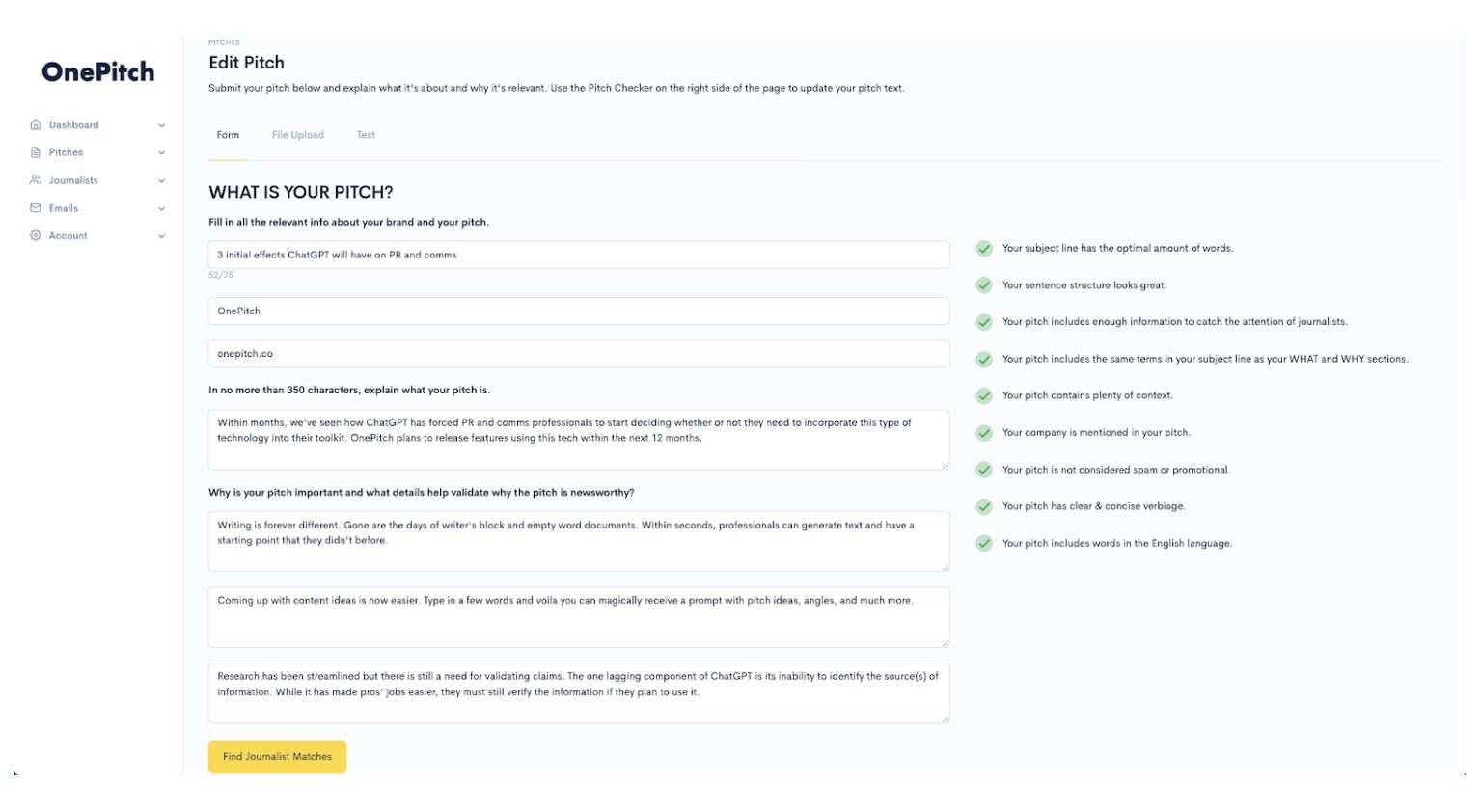
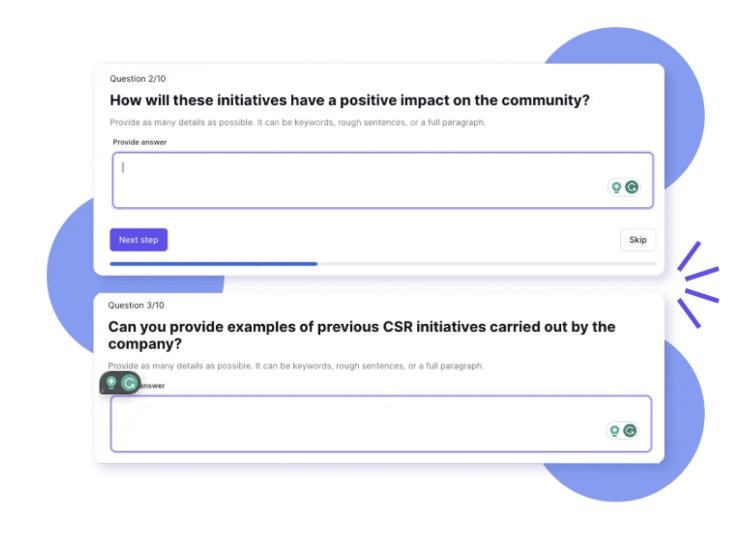
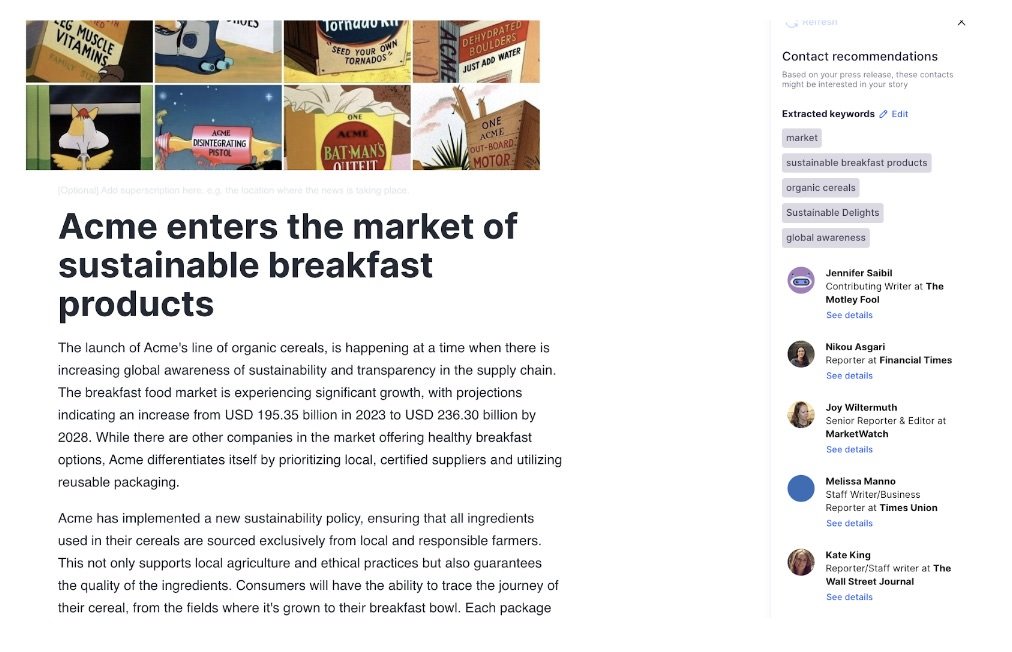
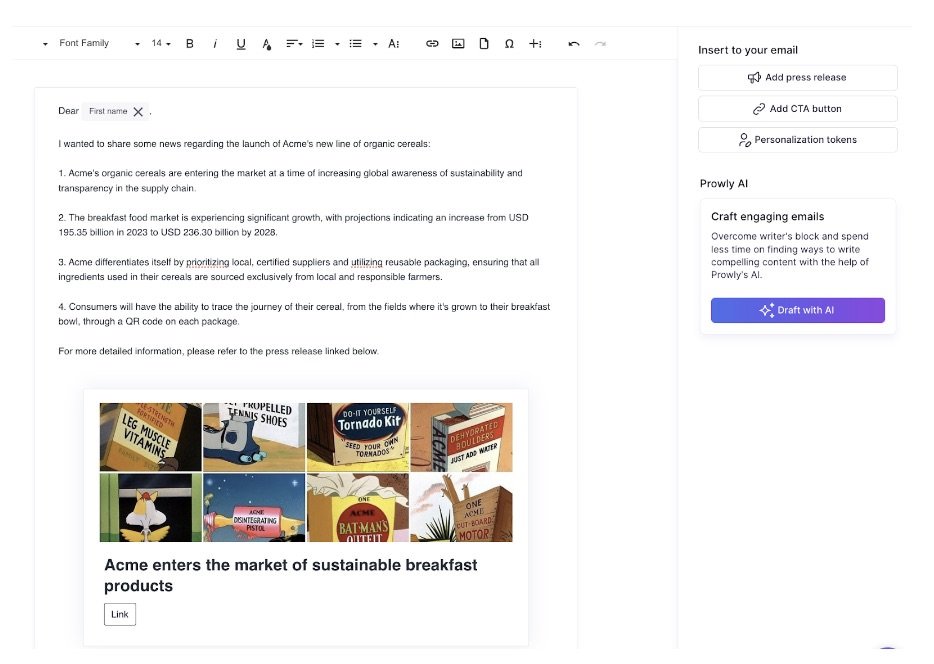
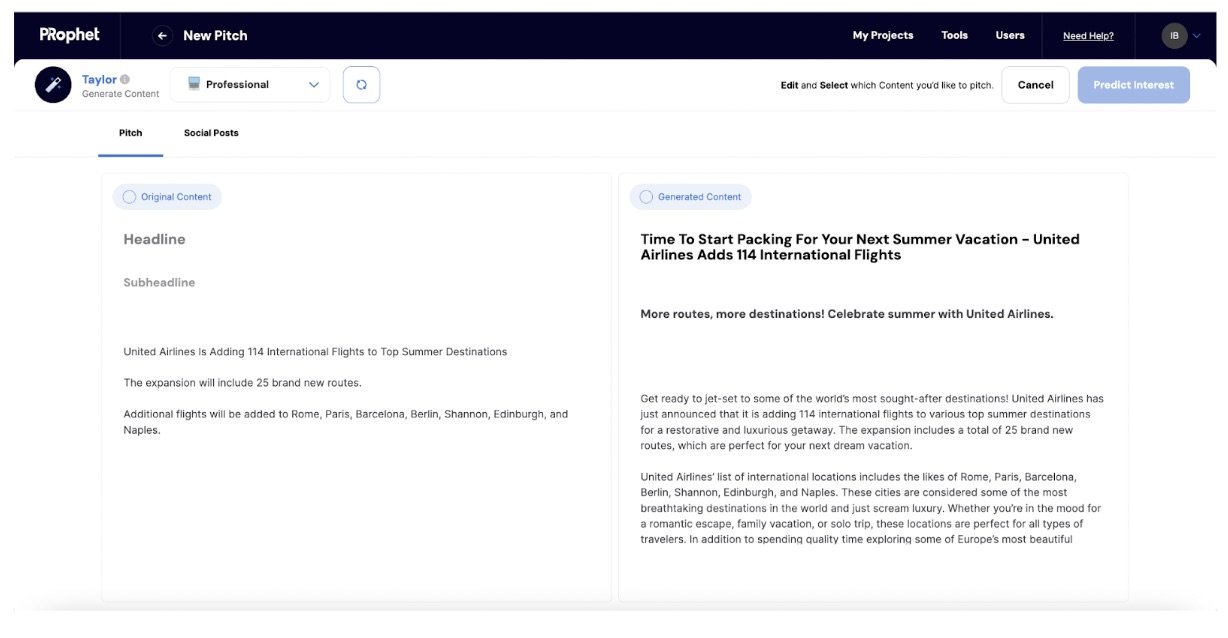
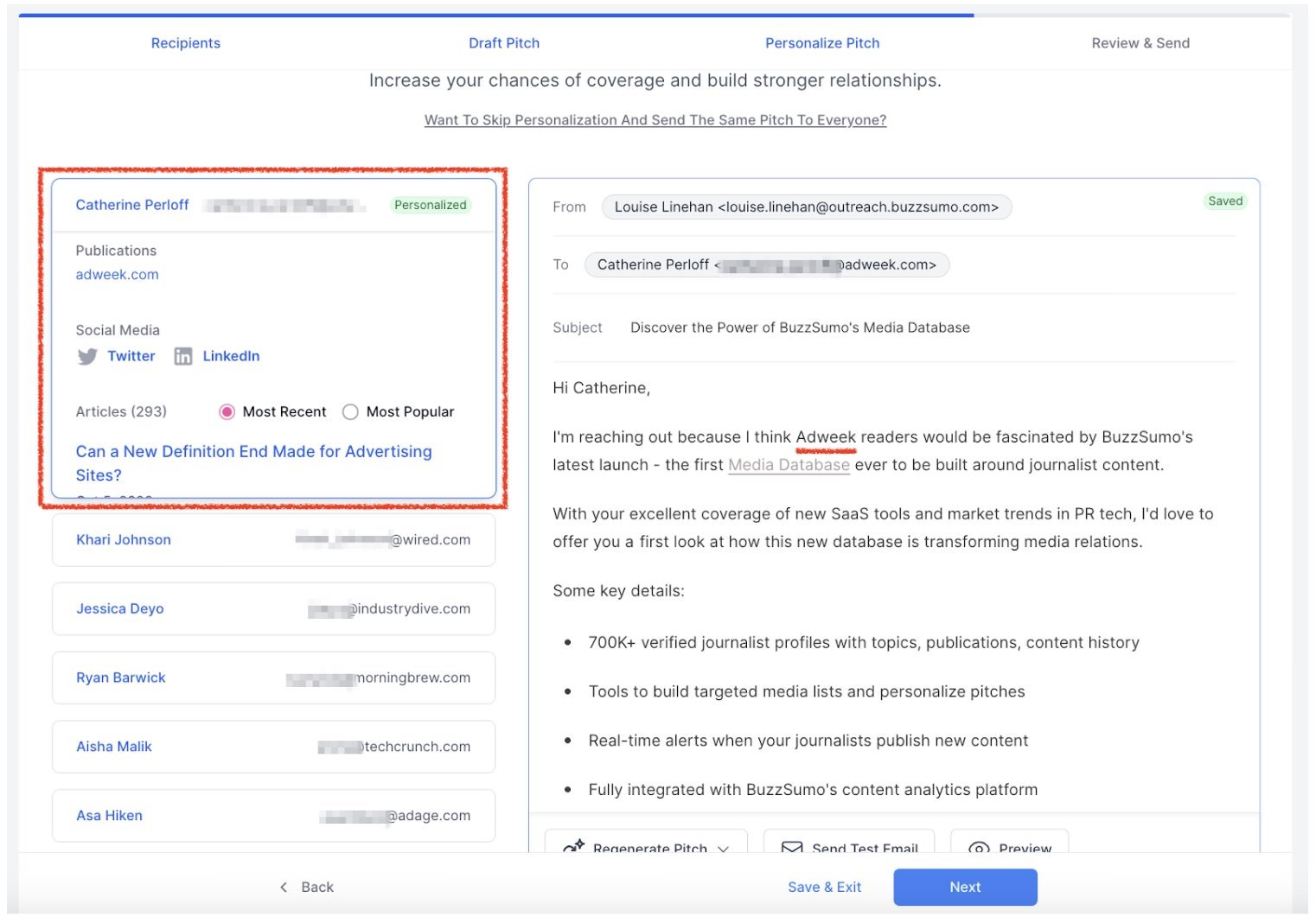
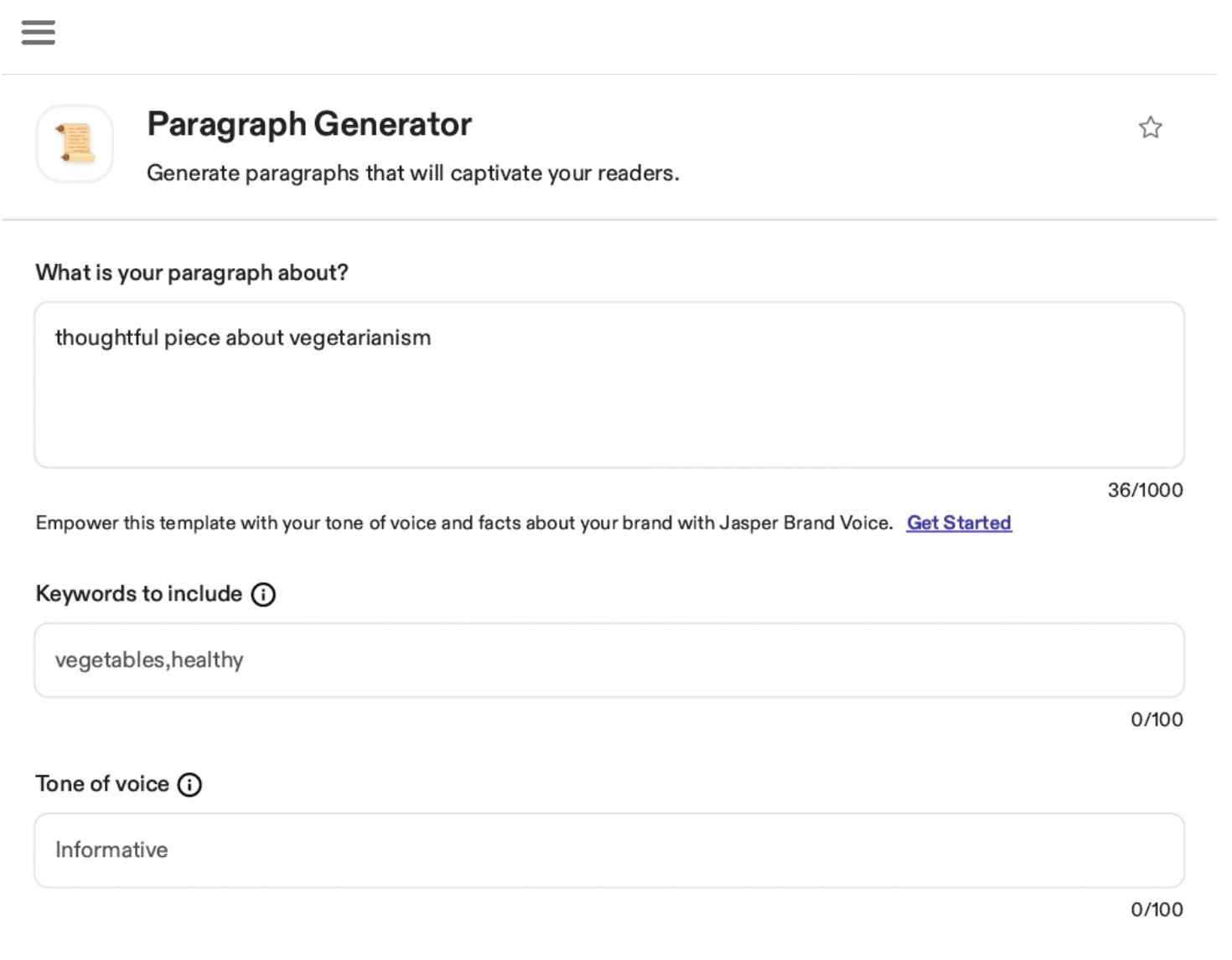
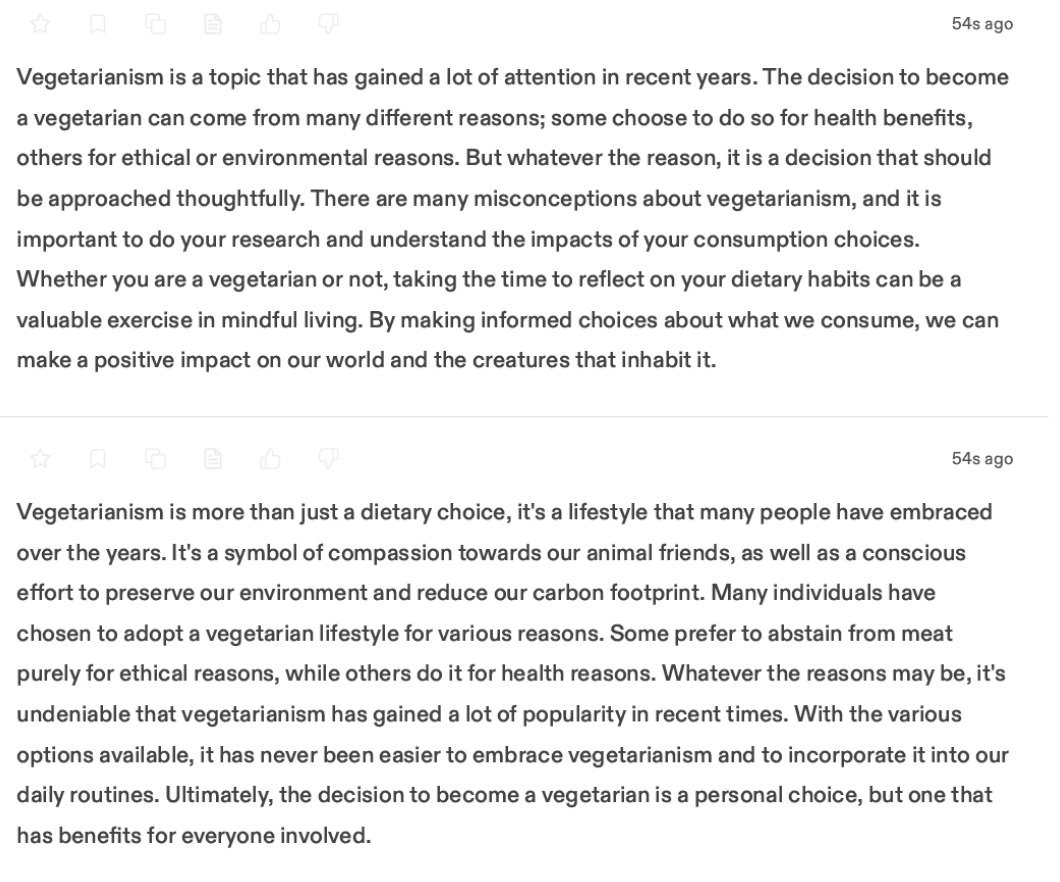
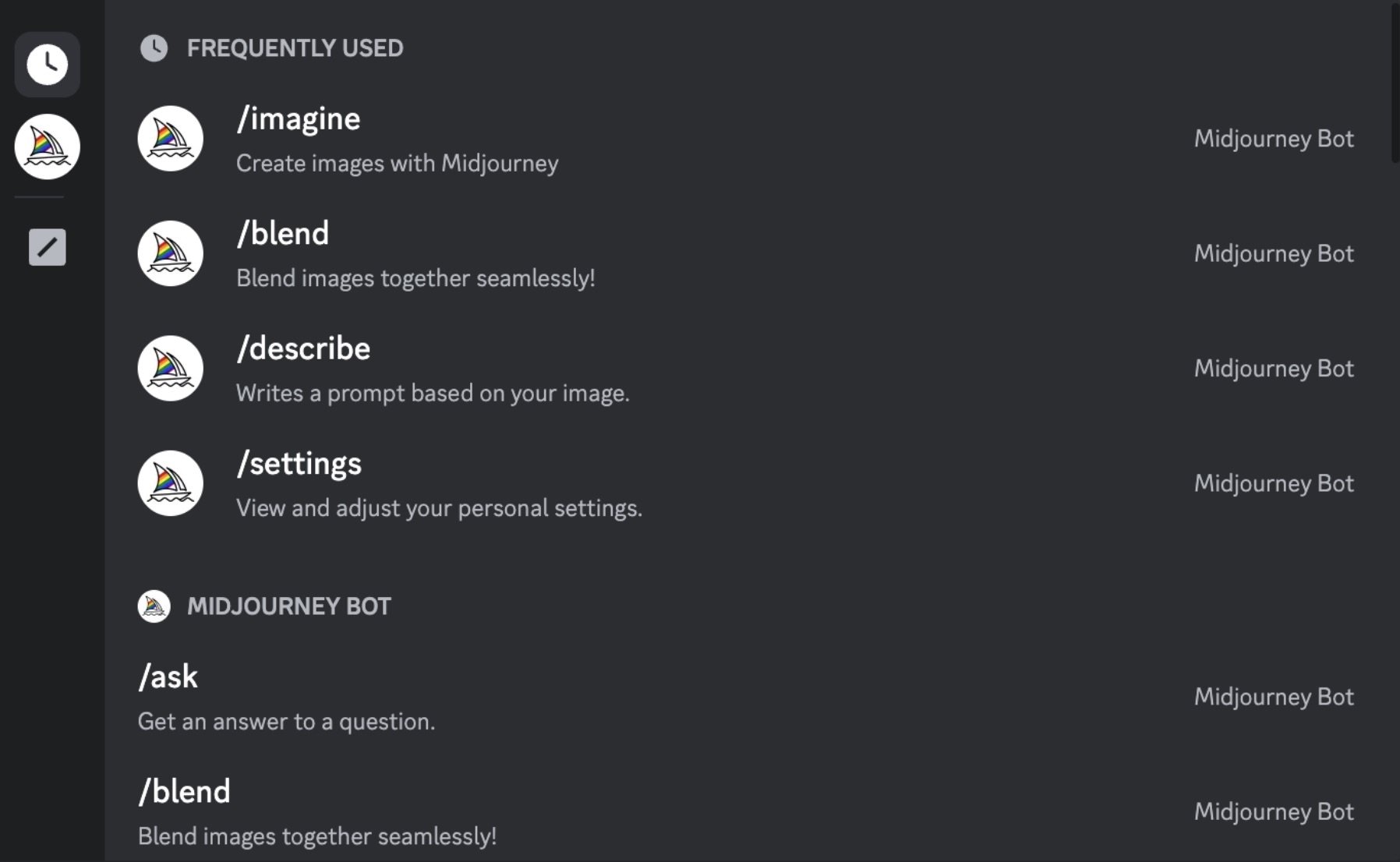
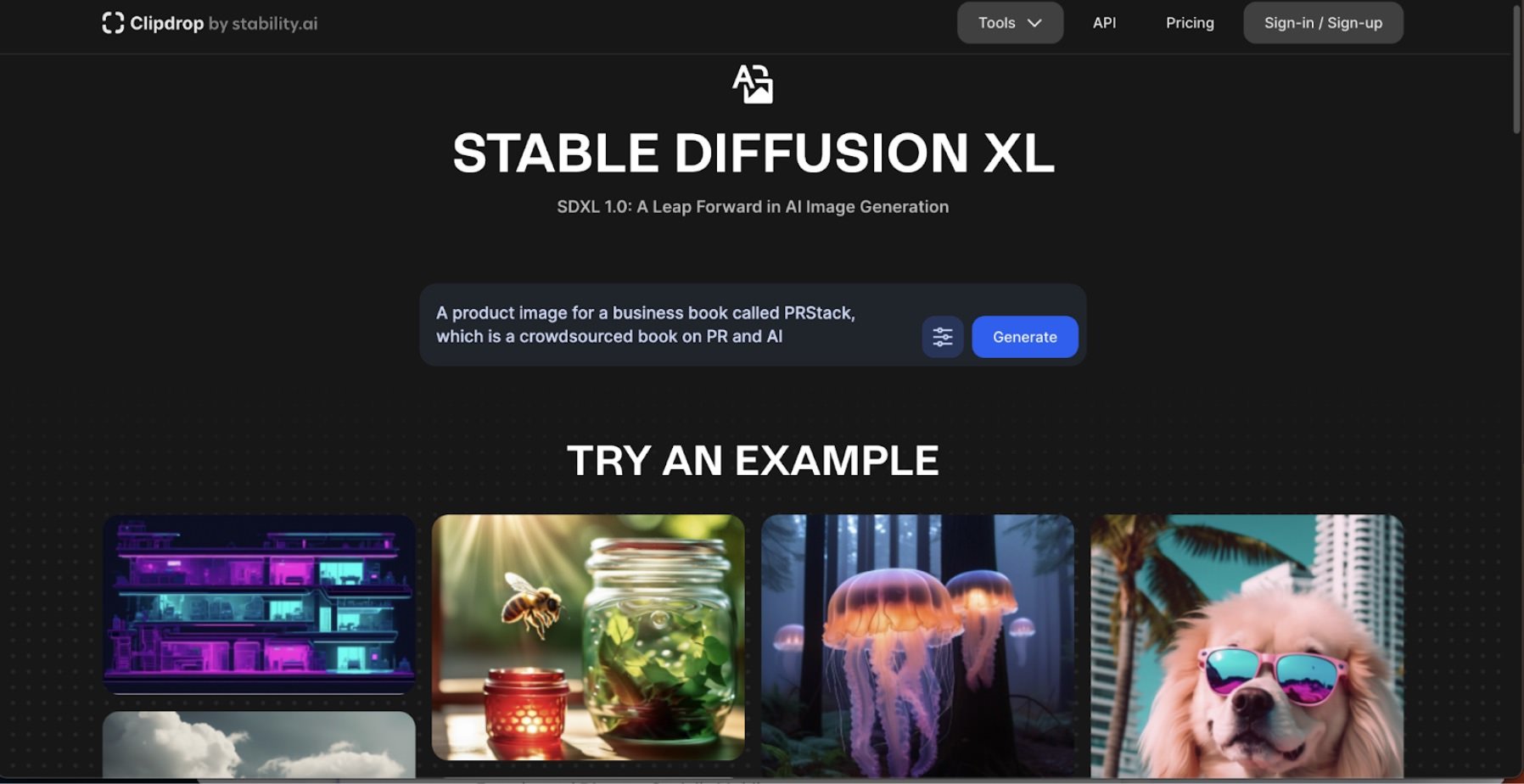
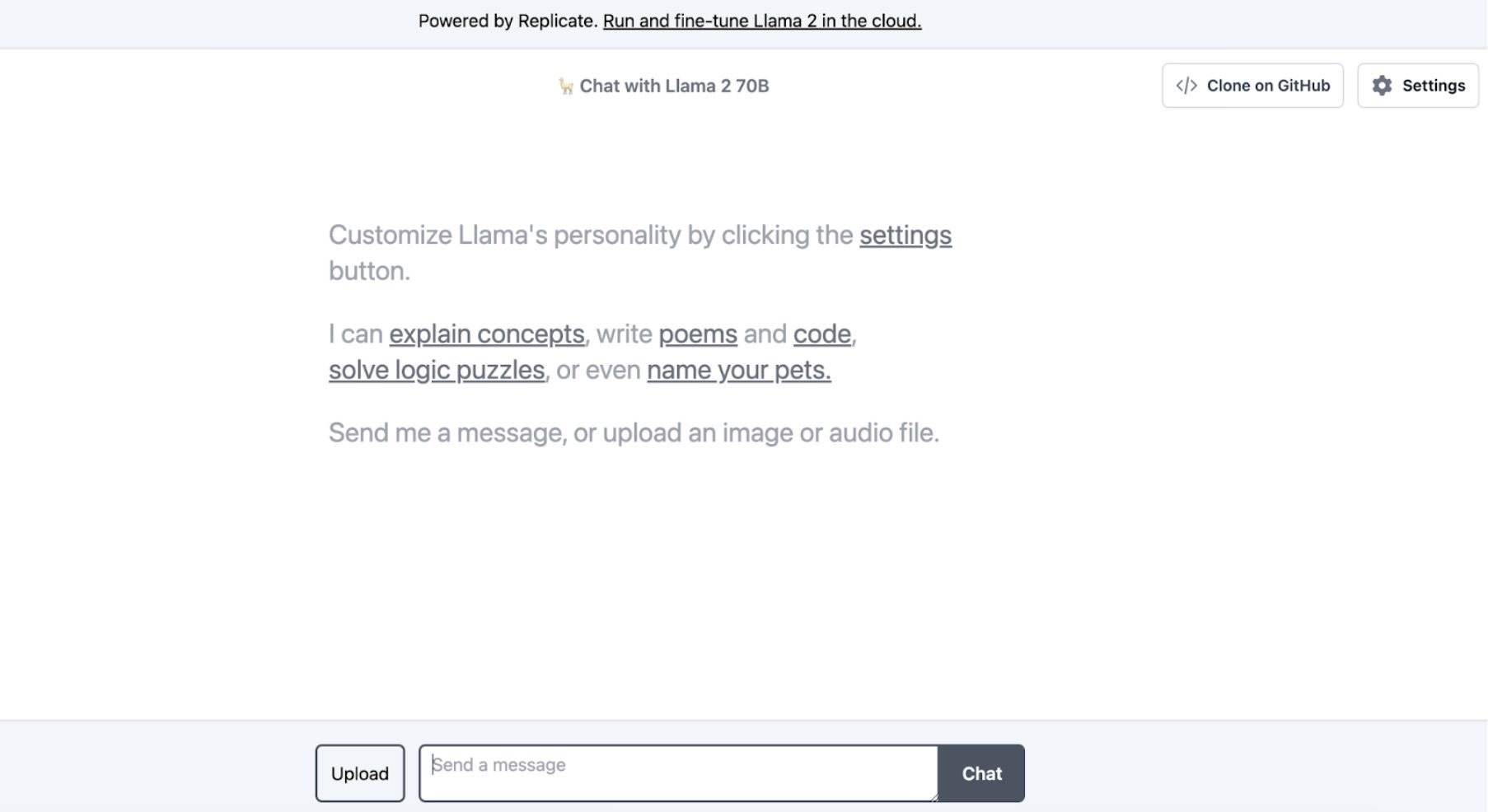
Using Propel is quite straightforward depending on what the objective is. To use the gen AI pitch, press release, and article writer, all a public relations practitioner needs to do is prompt the AI to get it to write a draft of what they want. Communicators can also input a draft pitch to get the AI to make a media list for them.
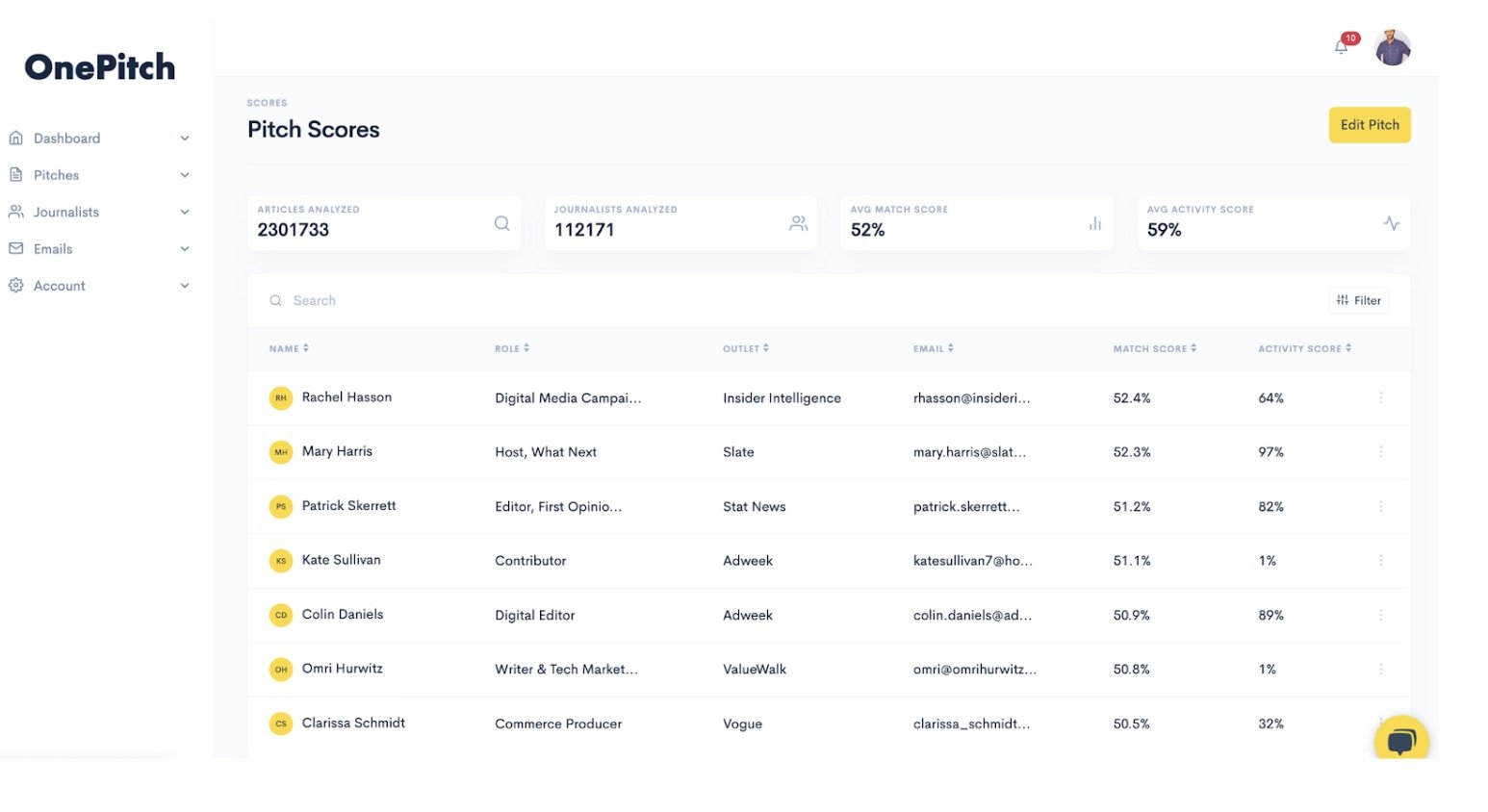
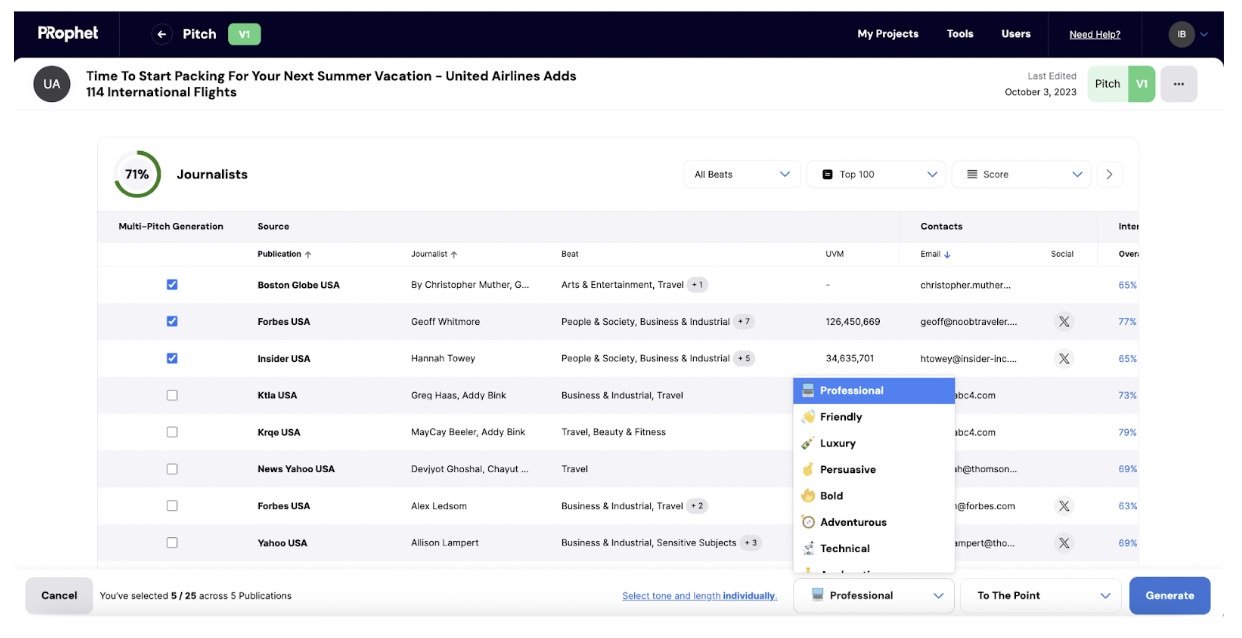
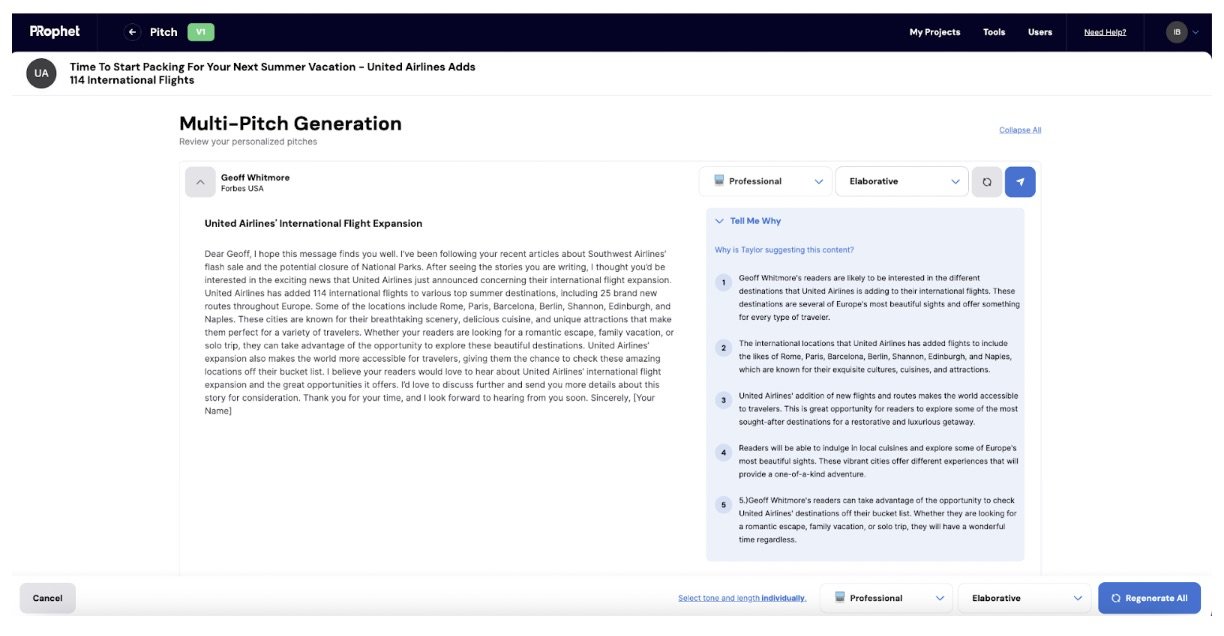
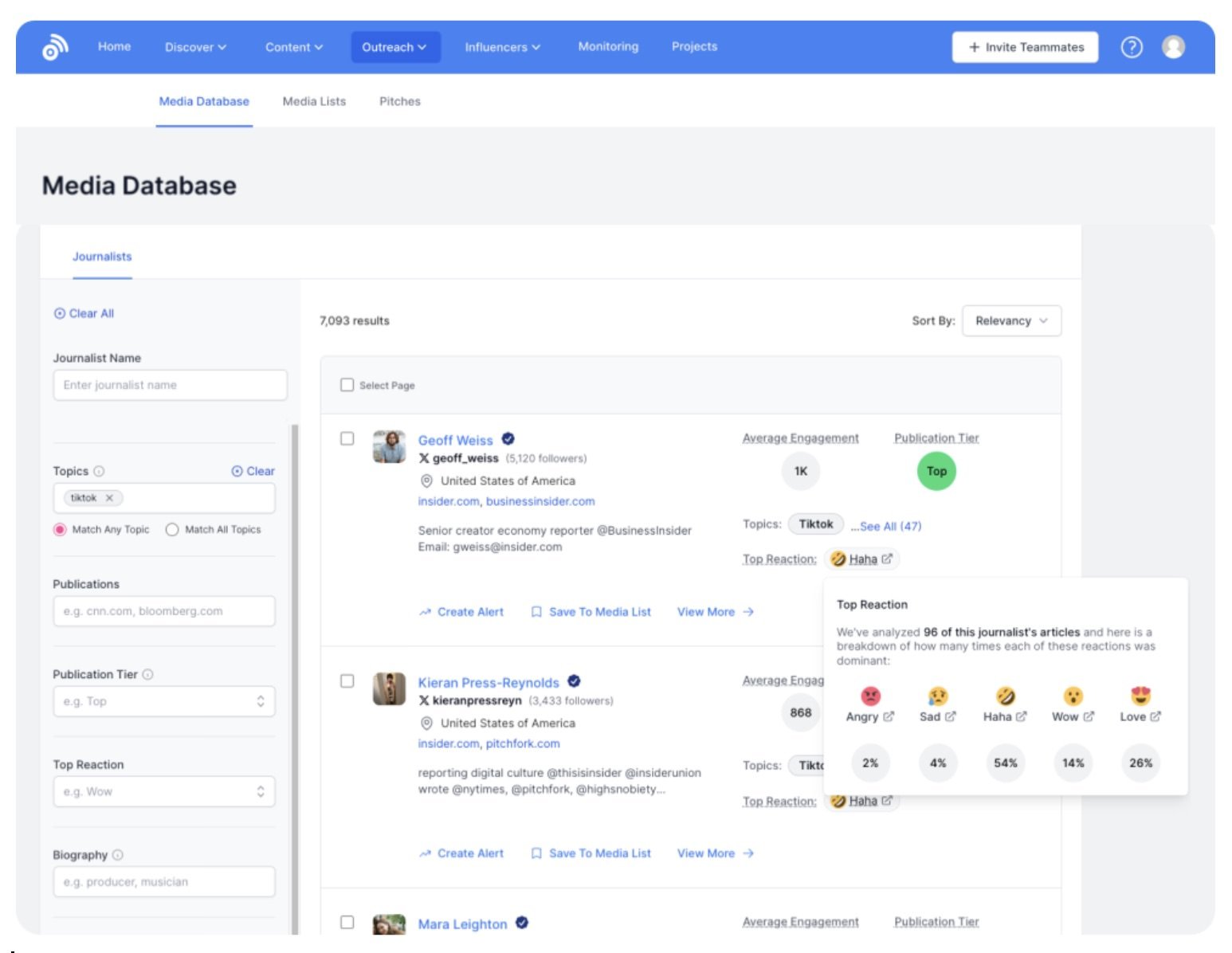
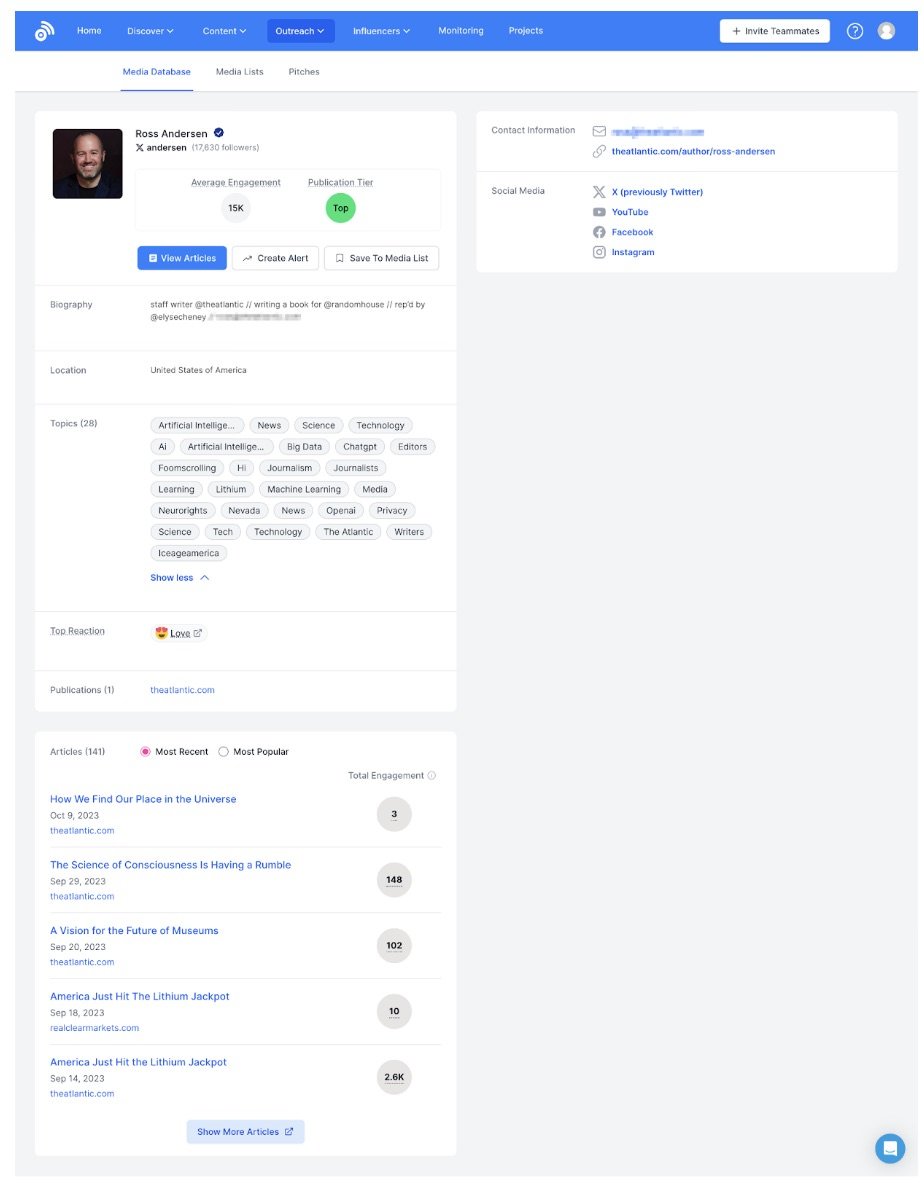
Propel’s journalist database is augmented by AI which can tell a media relations practitioner everything from what topics a journalist writes about, to open and response rates and even what day of the week and time they’re most likely to open a pitch. Communicators also have the option to create or add these journalists to media lists manually, as well as upload pre-made CSVs into the system.
To send a pitching campaign, all one needs to do is pull up the relevant media list inside their Gmail or Outlook, and then go through the list to determine who gets sent what. Upon hitting the PitchBooster button, the emails get saved to drafts, enabling communicators to tailor each pitch to each journalist.
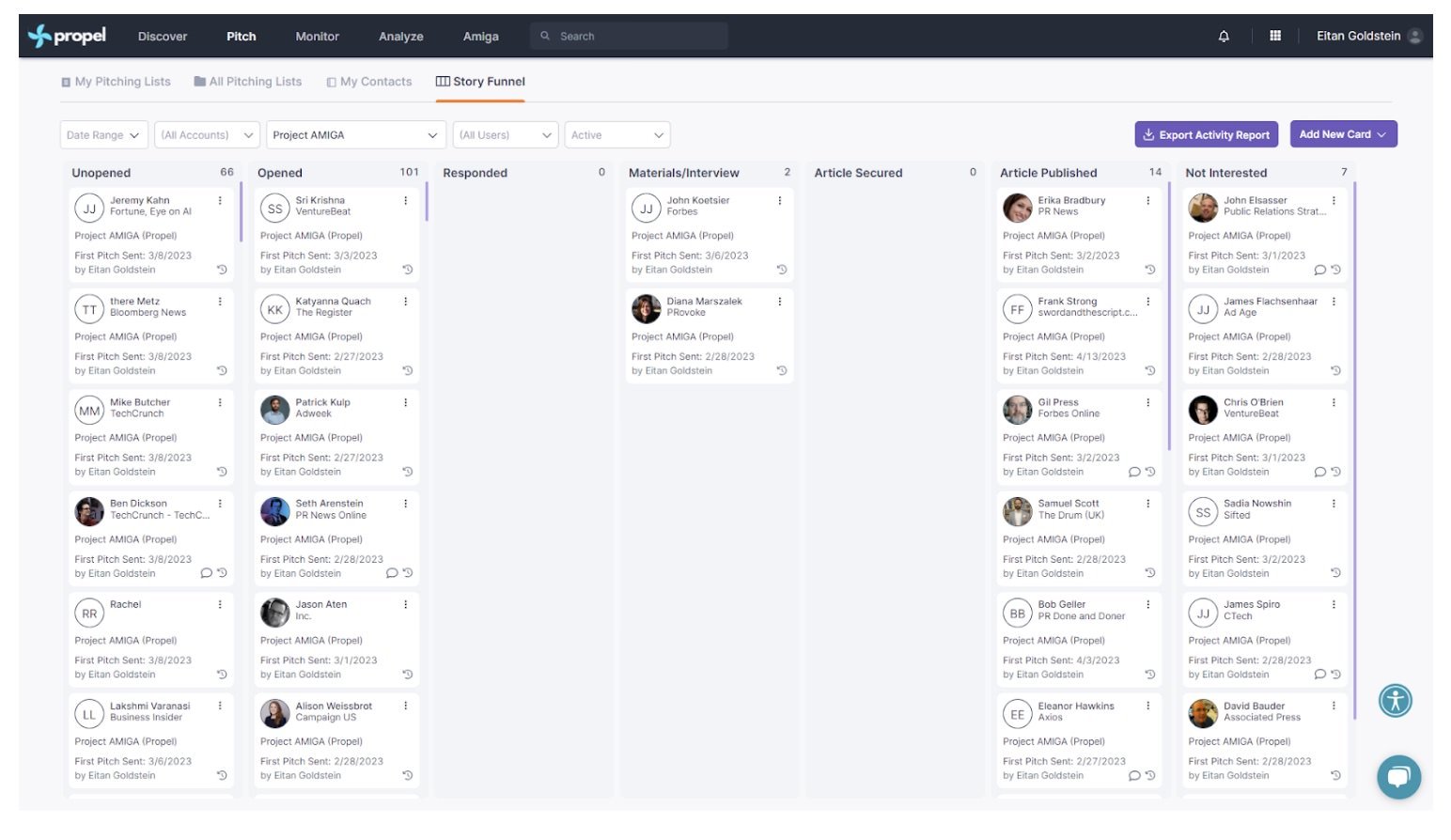
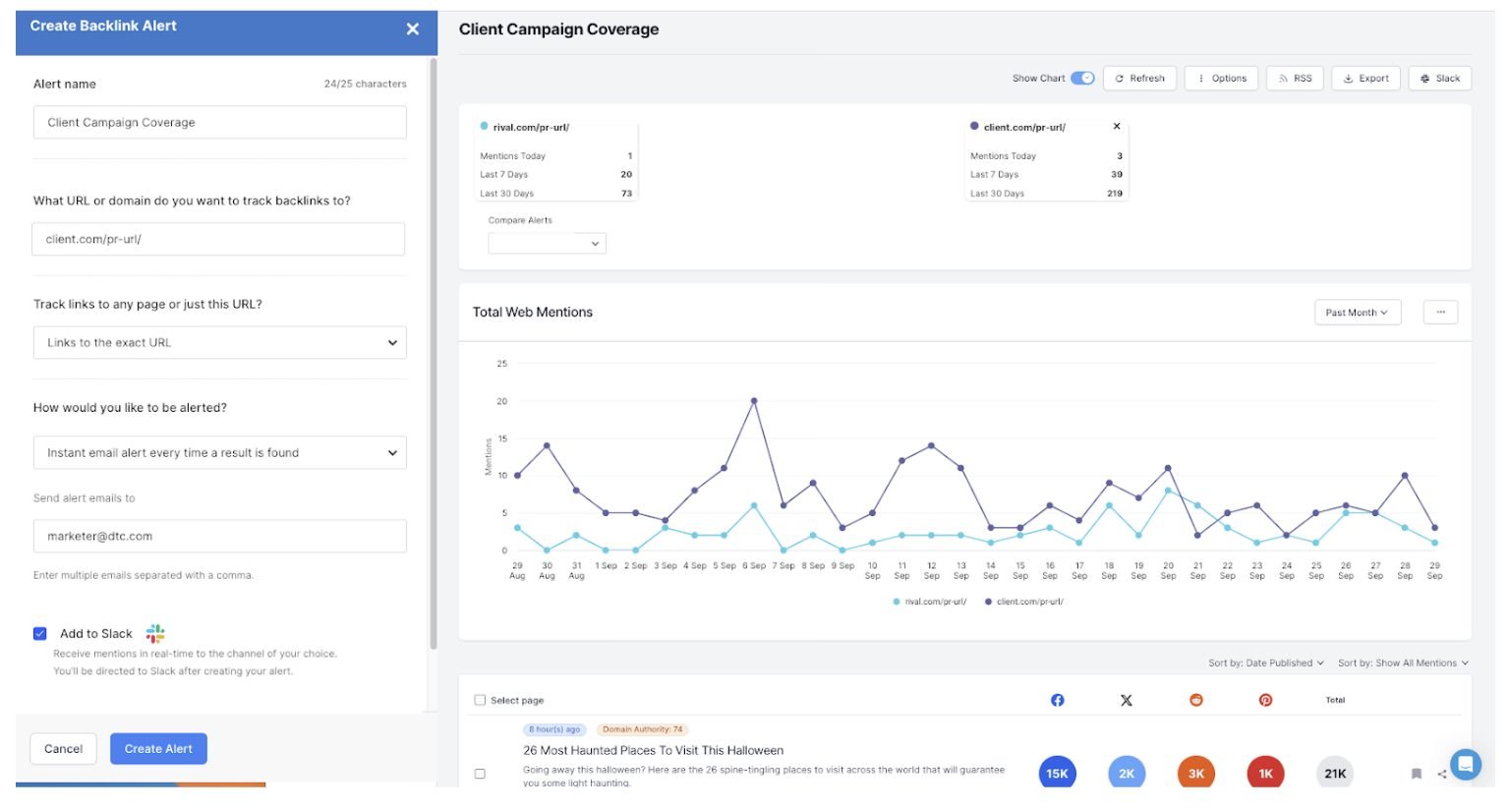
Once the pitch is sent, it’s automatically logged in the “story funnel.” As journalists begin asking for information, communicators can move the journalist tile along the funnel until the story is published. They can also write notes on the tile so everyone in the team can see if there are any special instructions.
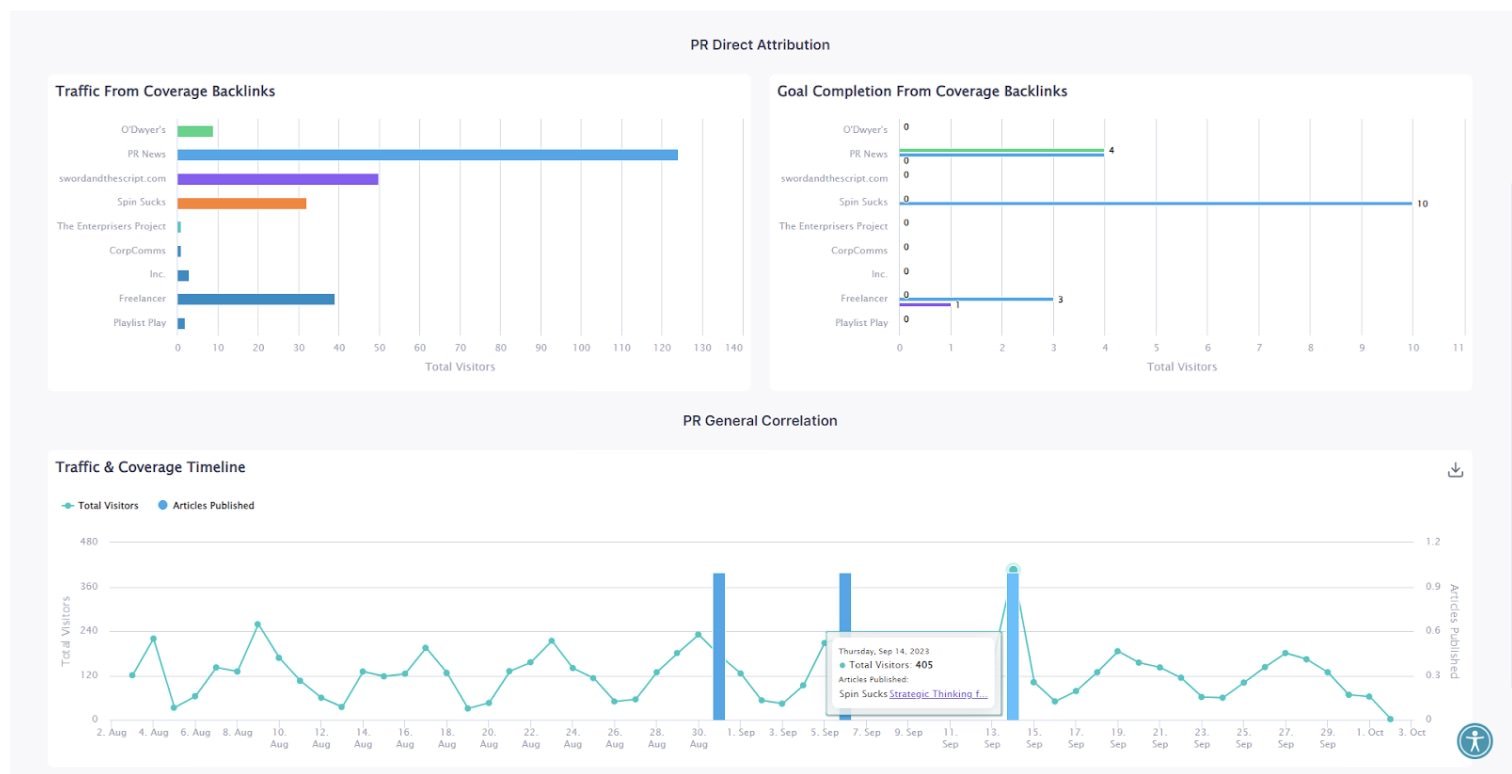
Finally, upon publication, the practitioner inputs the link to the story and Propel is automatically able to find the unique monthly visitors, title, author, etc of the article. This then ties into the organisation’s conversion metrics, enabling the organisation to see how many people enter their sales funnel from a particular piece of coverage.
Finally, upon publication, the practitioner inputs the link to the story and Propel is automatically able to find the unique monthly visitors, title, author, etc of the article. This then ties into the organisation’s conversion metrics, enabling the organisation to see how many people enter their sales funnel from a particular piece of coverage.
Zach Cutler, CEO, Propel
https://www.linkedin.com/in/zachc
Zach Cutler is the CEO of the fully accessible public relations platform Propel PRM and is one of the only VC-backed tech founders with a physical disability. Prior to this he owned and operated his own public relations agency - Cutler PR - for nine years and was the agency of record in the US for 70 tech start-ups.